Headaches are one of the most common complaints for which people consult a doctor (1). They can be episodic or chronic. The usual triggers can be stress, smoking, hunger, sleep problems, certain foods (such as chocolate, cheese and alcohol), the menstrual cycle and weather conditions (2). It is only when headaches are particularly severe or persistent, or cannot be treated by taking a painkiller, that most people go to the doctor. At this point, it is important for us to differentiate between the underlying causes of headaches.
Different types of headache
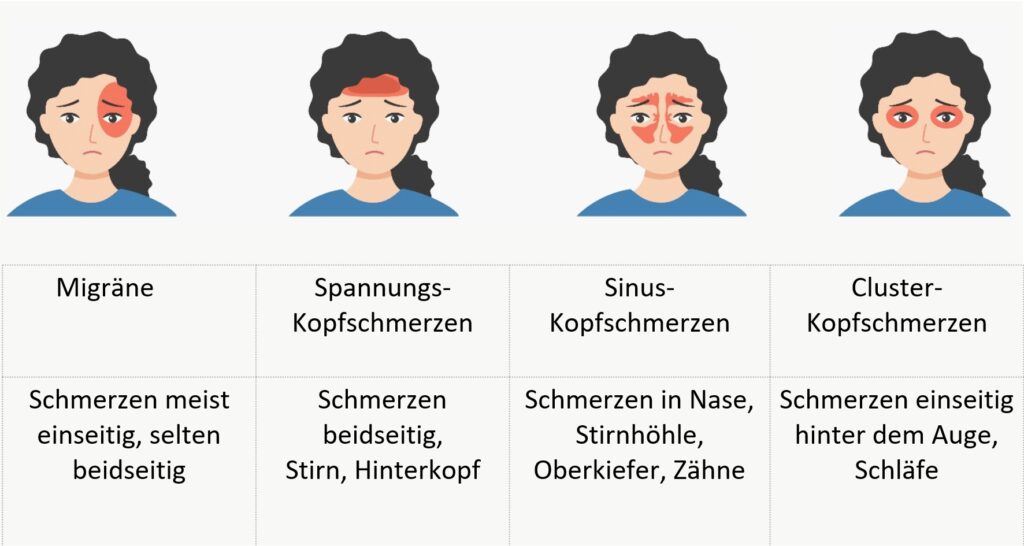
Migraine: major impact on quality of life
The second most common cause of headaches is migraine, which is often a massive burden on the patient’s quality of life.
A migraine is different from a normal headache, which almost everyone has from time to time. A migraine attack is characterized by the sudden onset of severe, stabbing pain, usually on one side of the head only. They are much more severe than normal headaches and are usually accompanied by other vegetative symptoms (such as visual disturbances, nausea, etc.). Longer migraine courses often lead to mixed symptoms of chronic migraine and tension headaches (3). Chronic headaches are defined as headaches lasting at least 15 days a month or more than 4 hours a day for three months. Women are more frequently affected, with the highest incidence occurring in the middle decades of life (around the age of 40).
Tension headaches: cooperation with the dental department is essential
Tension headache, which is the most common headache disorder, must be distinguished from this. This has a dull, pressing character and usually radiates over the entire head. The pathophysiology of tension headaches has not yet been sufficiently clarified. Increased tension in the neck muscles and the associated irritation of the nervous system are being discussed. Conventional medicine treats it with analgesics such as amitryptiline or NSAIDs such as ibuprofen. However, regular use of such painkillers can also lead to a so-called “drug-induced headache”. The
Pain can be triggered by hypersensitivity to the active ingredient as well as by an overdose or withdrawal. This so-called drug-induced headache very often occurs after the end of long-term treatment with analgesics. Since the use of conventional medicine usually does not achieve a satisfactory therapeutic result, a considerable proportion of patients seek complementary therapy methods (3).
In the case of tension headaches, we always work closely with the dental department at Paracelsus. There is a condition called Temporomandibular Joint Dysfunction (TMJ), which is often associated with jaw tension and headaches. The TMJ connects the jaw to the skull, and problems in this joint can cause pain that radiates to the head (4).
It is also possible that overactivity or tension of the jaw muscles due to teeth grinding or clenching (bruxism) can lead to headaches. In addition, poor tooth alignment, known as malocclusion, can cause stress on the jaw muscles and contribute to headaches. Finally, even dental problems such as cavities, infections or other dental issues can lead to referred pain that causes headaches. Therefore, effective treatment often requires collaboration between dentists, osteopaths and medical professionals to address the various aspects that contribute to jaw tension and headaches.
Sinus headache: understanding and effectively alleviating allergies
Sinus headaches, which are often caused by swelling of the mucous membranes in the sinuses or by allergies or chronic sinusitis, are classically characterized by a headache with a frontal emphasis. In most cases, bending the head forward leads to a worsening of symptoms. Patients often also suffer from other symptoms (seasonal allergic symptoms, sinus-bronchial syndrome, fatigue, etc.). These can also be accompanied by a dental focus, i.e. dental involvement.
This sinus headache clarification therefore also requires interdisciplinary cooperation with the dental clinic and can be detected by imaging (ultrasound or DVT diagnostics).
Cluster headache: Chronic with episodes
Cluster headaches, on the other hand, are one-sided, very severe attacks of head and facial pain that are localized and usually last between 15 and 180 minutes if left untreated. The main pain is in the area behind the eyes and in the forehead and temple region. To confirm the diagnosis, at least 5 attacks with at least one additional symptom (conjunctival redness, tearing of the eyes, swelling of the nose, runny nose, pupil constriction, drooping of the upper eyelid, swelling of the upper eyelid, sweating of the forehead and face) are defined. A basic distinction is made between episodic and chronic cluster headaches, with the majority suffering from episodic cluster headaches. The attacks often occur regularly at the same time of day, often in the first few hours after falling asleep or in the early morning.
Depending on the cause, it is also important to maintain a “holistic view” of the patient and also take into account secondary findings such as “allergies, dental status, posture, nutrition, stress regulation” in the treatment planning.
The assessment of the teeth and jaw tension, possibly so-called bruxism (teeth grinding) Particular attention is also paid to the assessment of teeth and jaw tension, so-called bruxism (teeth grinding), in the overall assessment (4). It is important to recognize and treat the signs as early as possible. Bruxism can occur during sleep and when awake. Around 20 percent of the population are affected. In addition to headaches, teeth clenching can also lead to tinnitus, tooth abrasion and other blockages (bruxism patients very often have a pelvic misalignment, for example).
Dental co-care, if necessary. Individually adapted flexible “splints”, targeted manual therapies, relaxation methods, MBSR and progressive muscle relaxation, for example, can lead to significant symptom relief.
Headache diagnosis for the best treatment strategy
The headache diagnosis can usually be determined on the basis of the patient’s medical history. To do this, it is important to keep detailed records and find out how long headache attacks last and what accompanying symptoms they are accompanied by. We scrutinize exactly what “triggers” there are, what “therapeutic measures” and treatments have been used so far against attacks and for prevention and to what extent these have been effective. By keeping a headache diary, sufferers can provide the doctor with valuable information about the course of the headache over time at the first contact. The doctor can recognize correlations and possible triggers. Examples include tyramine, which is found in wine and cheese, or nitrite from sausage products, caffeine, glutamate, etc. These vasoactive ingredients, everyday pollutants, need to be detected. In our experience at the Paracelsus Clinic, colon hydrotherapy provides immediate relief in this respect.
Some primary headache disorders, such as migraine, run in families, so information about the occurrence of headaches in the family is also important. A physical examination and a neurological examination are also an important basis for diagnosis. In individual cases, additional examinations may be carried out, such as a craniosacral and spinal assessment, dark field diagnostics, laboratory tests, measurement of heavy metal exposure, stool analysis, dental clarification or imaging (e.g. DVT, ultrasound, CT or MRI of the brain). For most headache disorders, magnetic resonance imaging (MRI) of the skull is preferable due to its good resolution and lack of radiation exposure; computer tomography (CT) is also used in emergency situations or for special questions.
Holistic therapy planning for headaches
Once the diagnostic procedures have been completed and the causes clarified, a holistic treatment plan can be drawn up. Complementary medical therapy plays an important role in the treatment of headaches:
Neural therapy in particular is an effective method for treating pain and various illnesses. By injecting small amounts of procaine (a local anaesthetic) and homeopathy, regulatory blockages in the body are removed and associated health disorders are supported in their self-healing process.
How does procaine work and why do we need an anesthetic? In the 1920s, the Huneke brothers discovered a way to use local anesthetics for therapeutic purposes as well as for local anesthesia. The “neural therapy according to Huneke” that they developed as a result is ideal for removing energy blockages in the tissue, because health means defense against harmful stimuli and requires an unhindered exchange of information. Neural therapy is a regulatory therapy like acupuncture or manual medicine and is now based on biological science. The application of neural therapy to an interference field can heal the disease caused by the interference field, as far as this is anatomically possible, via the seconds phenomenon. An interference field or focus is the point from which the disease originates, such as encapsulated bacterial colonies or old scars. Such interference fields are usually chronically stressful factors which themselves are inconspicuous and cause no symptoms, but which affect completely different regions of the body. Interference fields can permanently irritate bodily functions and weaken our natural defenses to such an extent that even minor stresses lead to malfunctions or pain that are often disproportionate to the trigger. If the patient is free of pain and symptoms immediately after the injection of the local anaesthetic, then the focus has been successfully localized and the body has been encouraged to regulate itself again during the anaesthetic seconds.

Headaches and nutrition
The nutritional approach to headache relief has been widely researched, with a plant-based diet having the best results (5).
In one study, the group with a plant-based diet showed a significant reduction in headache severity compared to a placebo group (5). The saturated fats in mainly animal products such as dairy products and meat had the greatest negative effect. Reducing the amount of fat in the diet to less than 30 grams per day led to a six-fold reduction in the frequency and intensity of headaches (6,7).
Even a moderately low-fat diet (less than 20% fat) showed significant decreases in headache frequency and severity. This suggests that reducing the intake of saturated fats, mainly in meat and dairy products, may help control migraine attacks. Green vegetables, rich in magnesium and other valuable compounds, may play a role in headache reduction. Magnesium supplements, although with no effect on severity, may reduce the frequency of migraine attacks (7,8).
It is advisable to include magnesium-rich foods such as green leafy vegetables, beans, nuts, seeds and whole grains in the diet. Magnesium supplements and magnesium infusions can also be considered, although ideally the nutrients should come from natural food sources.

Headaches and mind-body medicine
In addition to neural therapy and nutritional therapy, physical therapies (local heat treatments, manual therapies, etc.), orthomolecular medicine, classic naturopathic treatments and body-mind medicine have proven to be very effective in reducing the frequency and frequency of attacks. The strategies of body-mind medicine aim to support people in developing a healthy lifestyle in their everyday lives (9). Particular attention is paid to the reciprocal influence of mind, psyche, body and behavior on health (10,11).
The roots of MBM lie, among other things, in the results of stress research, supporting people in developing and maintaining the ability to care for themselves. MBM can also offer support in finding meaning in one’s own life and current life situation. Thus, in addition to conventional and naturopathic medicine, body-mind medicine offers a resource-oriented therapy that supports the patient in their own activity to consciously participate in their own recovery and the maintenance of their health. The identification of stressors and triggers is suitable for the treatment of tension headaches. Stress management through mindfulness (Mindfulness-Based Stress Reduction Program – MBSR), movement therapy, meditation, bio-feedback, kinesiology, progressive muscle relaxation, hydrotherapy and other therapies (12). For migraine patients, it is also very important to ensure adequate sleep duration, daily rhythms and avoidance of noxious substances (coffee, alcohol and smoking).
In individual cases, a complex inpatient multimodal therapy measure may also be useful initially.
In addition to balanced lifestyle modification and dietary changes, orthomolecular methods (procaine, magnesium, mineral infusions), targeted phytotherapy, manual therapies and targeted heat therapies (e.g. Indiba and Papimi) have also proven effective. TCM and acupuncture are also used in addition to neural therapy. At the Paracelsus Clinic, patients are always assessed individually and a treatment plan is drawn up accordingly.
Overall, there is a growing interest in biological medicine and a holistic approach to the treatment of headaches. Rather than just alleviating the symptoms, biological medicine focuses on root cause research and aims to identify the underlying triggers. Through a comprehensive analysis of medical history, headache diaries and diagnostic procedures, individualized treatment plans can be developed that include both conventional and complementary approaches. Our short-term goal is to find a combination of methods that successfully reduce the frequency and severity of attacks. However, by integrating biological medicine and holistic treatment approaches, it is hoped that patients with headaches and migraines can experience long-term relief and an improved quality of life.
References:
1 Ha H, Gonzalez A. Migraine Headache Prophylaxis. Am Fam Physician. 2019;99(1):17-24.
2 Bega D. Complementary and Integrative Interventions for Chronic Neurologic Conditions Encountered in the Primary Care Office. Prim Care. 2017;44(2):305-322.
3 Huber R., Michalsen A. 2014; Checklist Complementary Medicine. Haug Verlag 372-382.
4 Matheson EM, Fermo JD, Blackwelder RS. Temporomandibular Disorders: Rapid Evidence Review. Am Fam Physician. 2023 Jan;107(1):52-58.
5 Jain MM, Kumari N, Rai G. A novel formulation of veggies with potent anti-migraine activity. Int J Comput Biol Drug Des. 2015;8(1):54-61.
6 Hindiyeh N, Aurora SK. What the Gut Can Teach Us About Migraine. Curr Pain Headache Rep. 2015;19(7):33.
7 Bunner AE, Agarwal U, Gonzales JF, Valente F, Barnard ND. Nutrition intervention for migraine: a randomized crossover trial. J Headache Pain. 2014;15:69.
8 Bic Z, Blix GG, Hopp HP, Leslie FM, Schell MJ. The influence of a low-fat diet on incidence and severity of migraine headaches. J Womens Health Gend Based Med. 1999;8(5):623-30.
9 Ferrara LA, Pacioni D, Di fronzo V, et al. Low-lipid diet reduces frequency and severity of acute migraine attacks. Nutr Metab Cardiovasc Dis. 2015;25(4):370-5.
10 Pfaffenrath V, Wessely P, Meyer C, et al. Magnesium in the prophylaxis of migraine–a double-blind placebo-controlled study. Cephalalgia. 1996;16(6):436-40.
11 Veronese N, Demurtas J, Pesolillo G, et al. Magnesium and health outcomes: an umbrella review of systematic reviews and meta-analyses of observational and intervention studies. Eur J Nutr. 2019;
12 Erwin Wells R, Phillips RS, McCarthy EP. Patterns




